The Promising Potential of EphA3-Specific CAR T Cells
Glioblastoma multiforme (GBM) is an extremely aggressive form of brain cancer that affects both children and adults. Current treatment options for GBM, such as surgery, radiation, and chemotherapy, have limited effectiveness, and the prognosis for patients remains very poor. The median survival time is just over one year, highlighting the crucial need for new and innovative therapies.
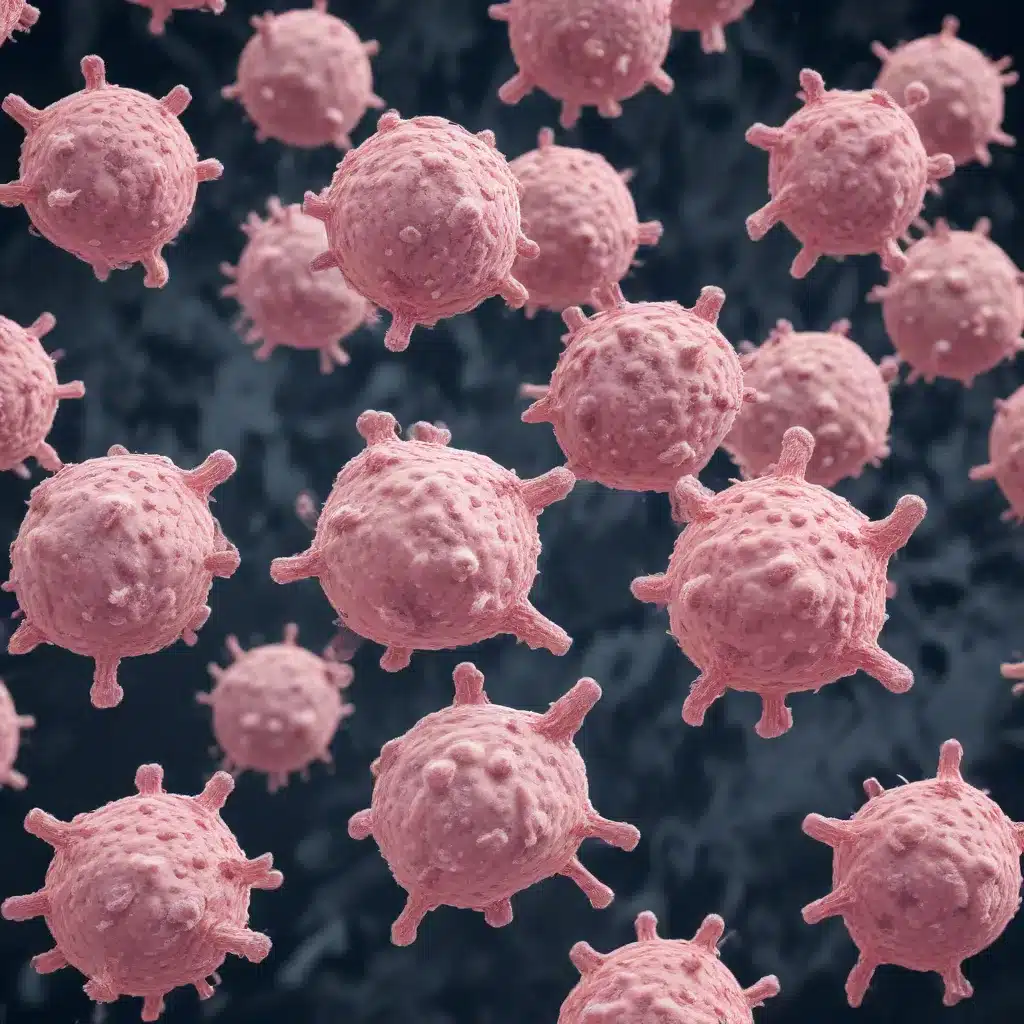
One promising approach that has generated significant interest is the use of chimeric antigen receptor (CAR) T cell therapy. CAR T cells are a type of immunotherapy where a patient’s own T cells are genetically engineered to express a receptor that recognizes a specific protein on the surface of cancer cells. When these CAR T cells are infused back into the patient, they can identify and destroy the targeted cancer cells.
CAR T cell therapy has achieved remarkable success in treating certain blood cancers, but its application in solid tumors like GBM has been more challenging. Researchers are continuously working to overcome the unique obstacles presented by solid tumors, including the hostile tumor microenvironment, limited T cell trafficking and infiltration, and the heterogeneity of target antigen expression.
One particularly promising target antigen for GBM is EphA3, a receptor tyrosine kinase that is highly expressed in many solid tumors, including GBM, but has limited expression in healthy adult tissues. Preclinical studies have shown that EphA3-specific CAR T cells can effectively eliminate GBM cells, both in vitro and in animal models, without causing significant toxicity to normal tissues.
In this article, we will explore the potential of EphA3-targeted CAR T cell therapy for the treatment of GBM. We will discuss the key features of EphA3 that make it an attractive target, the preclinical evidence supporting the use of EphA3-specific CAR T cells, and the ongoing clinical trials investigating this approach. Additionally, we will examine the strategies being developed to enhance the efficacy and safety of EphA3-targeted CAR T cell therapy for GBM.
The Unique Challenges of Treating Glioblastoma
GBM is the most common and aggressive type of primary brain cancer in adults. The standard treatment approach typically involves surgical resection, followed by radiation therapy and chemotherapy with the drug temozolomide. However, the prognosis for GBM patients remains dismal, with a median overall survival of just 12-15 months, and a 5-year survival rate of less than 5%.
One of the key challenges in treating GBM is the highly heterogeneous nature of the tumor. GBM tumors are composed of a diverse population of cells, including differentiated tumor cells, cancer stem-like cells, and cells that have undergone epithelial-to-mesenchymal transition. This heterogeneity allows the tumor to adapt and evolve, making it resistant to traditional therapies.
Another major obstacle is the location of the tumor within the brain. The blood-brain barrier, which normally protects the brain from harmful substances, can also prevent effective delivery of many cancer therapies, including chemotherapeutic drugs and even some immunotherapies. This makes it difficult to achieve sufficient concentrations of the therapeutic agents at the tumor site.
Additionally, the tumor microenvironment in GBM is highly immunosuppressive, with the presence of various inhibitory immune cells, such as regulatory T cells and myeloid-derived suppressor cells, as well as the expression of immune checkpoint molecules like PD-L1. This creates a hostile environment that can impair the function and infiltration of anti-tumor immune cells, including CAR T cells.
Targeting EphA3 with Chimeric Antigen Receptor T Cells
EphA3 is a member of the Eph receptor tyrosine kinase family, which play crucial roles in various developmental processes, including tissue patterning, cell migration, and angiogenesis. In healthy adult tissues, EphA3 expression is generally low, with the highest levels found in the uterus, bladder, and prostate.
However, EphA3 is frequently overexpressed in a wide range of solid tumors, including GBM, where it is often associated with a more aggressive, mesenchymal phenotype and the presence of progenitor or stem-like tumor cells. Elevated EphA3 expression has also been linked to poorer patient outcomes in many cancer types.
The restricted expression of EphA3 in normal adult tissues, coupled with its prominent role in GBM progression, makes it an attractive target for CAR T cell-based immunotherapy. Preclinical studies have demonstrated that EphA3-specific CAR T cells can effectively recognize and eliminate EphA3-positive GBM cells, both in vitro and in animal models.
One key advantage of targeting EphA3 with CAR T cells is that the recognition and killing of cancer cells is independent of MHC class I presentation, which can be disrupted in many GBM tumors. This helps to overcome a common immune evasion mechanism employed by GBM cells.
Preclinical Evidence for EphA3-Targeted CAR T Cells
Researchers have developed EphA3-specific CAR T cells using an scFv (single-chain variable fragment) derived from the EphA3-targeting antibody ifabotuzumab. These CAR T cells have shown promising results in preclinical studies:
-
In vitro cytotoxicity: EphA3-specific CAR T cells were able to effectively recognize and kill GBM cell lines expressing EphA3, demonstrating potent anti-tumor activity.
-
Targeting GBM stem-like cells: EphA3-positive GBM stem-like cells, which are often resistant to conventional therapies, were also recognized and eliminated by the EphA3-specific CAR T cells.
-
Inhibition of tumor growth: In orthotopic GBM xenograft models, administration of EphA3-specific CAR T cells resulted in significant inhibition of tumor growth and prolonged survival of the mice, compared to control treatments.
-
Tumor localization and safety: Positron emission tomography (PET) imaging studies using the EphA3-targeting antibody ifabotuzumab have shown excellent tumor localization with minimal normal tissue uptake, suggesting a potential safety profile for EphA3-targeted therapies.
These promising preclinical results have led to the initiation of several clinical trials investigating the use of EphA3-targeted CAR T cells for the treatment of GBM and other solid tumors.
Ongoing Clinical Trials with EphA3-Specific CAR T Cells
Building on the preclinical data, researchers have begun to translate EphA3-targeted CAR T cell therapy into the clinic for the treatment of GBM and other solid malignancies.
One notable clinical trial is the Phase 1 study (NCT03386903) evaluating the safety and efficacy of EphA3-specific CAR T cells in patients with recurrent or refractory GBM. In this trial, patients will receive a single dose of the CAR T cells, either by direct injection into the tumor resection cavity or by intraventricular administration.
Another ongoing trial (NCT03374943) is investigating the use of the EphA3-targeting antibody ifabotuzumab for imaging and targeting of GBM tumors. This study aims to assess the safety and tumor-targeting ability of the ifabotuzumab antibody, which could pave the way for the development of EphA3-targeted therapies, including CAR T cells.
These clinical trials will provide critical insights into the safety, feasibility, and potential efficacy of EphA3-targeted CAR T cell therapy for the treatment of GBM. If successful, this approach could represent a significant advancement in the management of this devastating disease.
Strategies to Enhance EphA3-Targeted CAR T Cell Therapy
While the initial preclinical data on EphA3-specific CAR T cells are promising, researchers are continuously working to optimize and improve this approach to overcome the unique challenges associated with treating solid tumors like GBM.
One key strategy is to combine EphA3-targeted CAR T cells with other therapeutic modalities, such as:
-
Immune checkpoint blockade: Incorporating anti-PD-1 or anti-CTLA-4 antibodies can help reinvigorate the function of CAR T cells and overcome the immunosuppressive tumor microenvironment.
-
Oncolytic viruses: Engineered viruses that selectively infect and lyse tumor cells can help create a more favorable environment for CAR T cell infiltration and activity.
-
Chemotherapy and radiation: Combining CAR T cell therapy with standard-of-care treatments can sensitize tumor cells, enhance antigen presentation, and improve the trafficking and persistence of CAR T cells.
Another approach is to further engineer the CAR construct to improve the functionality and safety of the EphA3-targeted CAR T cells. This includes strategies such as:
-
Incorporating cytokine secretion: Equipping the CAR T cells with the ability to secrete cytokines like IL-15 can enhance their proliferation, persistence, and anti-tumor activity.
-
Utilizing dual-targeting CARs: Designing CAR T cells that recognize two distinct antigens, such as EphA3 and another GBM-associated target, can help overcome the issue of antigen heterogeneity.
-
Implementing safety switches: Incorporating inducible safety mechanisms, such as suicide genes, can allow for better control and management of potential adverse events.
By leveraging these innovative strategies, researchers aim to maximize the therapeutic potential of EphA3-targeted CAR T cell therapy and improve outcomes for patients with GBM.
Conclusion: Unlocking the Promise of EphA3-Targeted Immunotherapy
The development of EphA3-specific CAR T cell therapy represents a promising approach in the fight against glioblastoma multiforme (GBM). The restricted expression of EphA3 in normal adult tissues, coupled with its prominent role in GBM progression, makes it an attractive target for this innovative immunotherapeutic strategy.
Preclinical studies have demonstrated the ability of EphA3-targeted CAR T cells to effectively recognize and eliminate GBM cells, including cancer stem-like cells, without significant toxicity to healthy tissues. These promising results have led to the initiation of several clinical trials that will further evaluate the safety and efficacy of this approach in patients with GBM.
As researchers continue to refine and optimize EphA3-targeted CAR T cell therapy, they are exploring various strategies to enhance its potency and safety, such as combining it with other therapies, engineering the CAR construct, and implementing safety switches. These advancements hold the potential to unlock new frontiers in the treatment of this devastating brain cancer.
The Stanley Park High School community remains committed to supporting innovative cancer research and providing the latest updates to our students and families. We are excited to follow the progress of EphA3-targeted CAR T cell therapy and its impact on improving outcomes for patients with glioblastoma multiforme.

