The Rise of Digital Pathology in Education
Digital pathology (the technology whereby glass histology slides are scanned at high resolution, digitised, stored and shared with pathologists, who can view them using microscopy software on a screen) is transforming the delivery of clinical diagnostic pathology services around the world. In addition to adding value to clinical histopathology practice, digital histology slides provide a versatile medium to achieve the educational needs of a variety of learners including undergraduate students, postgraduate doctors in training and those pursuing continuing professional development portfolios.
In this guide, we will review the principal use cases for digital slides in training and education and share tips for successful use of digital pathology to support a range of learners. This is based on experience gathered at Leeds Teaching Hospitals National Health Service Trust and the National Pathology Imaging Co-Operative during the last 5 years of digital slide usage.
Advantages of Digital Slides in Histopathology Education
Traditionally, histopathology education has been delivered using glass slides, conventional light microscopy and physical textbooks with static photographs of classic disease presentations. Teaching sets of glass slides are accrued by universities and clinical departments, and shared with students, who view the slides on individual microscopes or via a multi-headed microscope with a trainer. Many of these slides are unique training resources, containing precious patient tissue that cannot be recut or duplicated, which places major constraints on the availability and transferability of the slides.
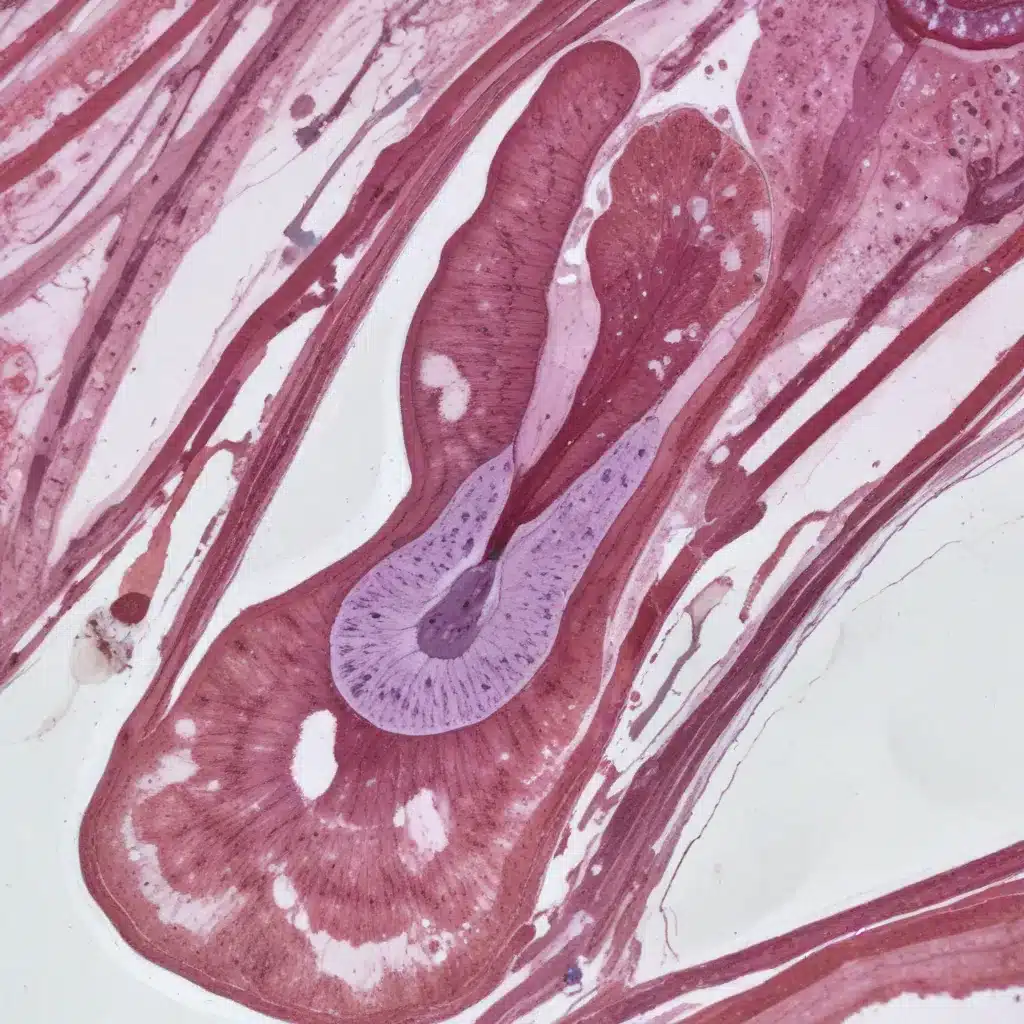
Use of a conventional light microscope requires practice, experience and development of core visual and motor skills, and can form a stumbling block for efficient histopathology education of a novice microscopist. A digital slide, on the other hand, contains digital information equivalent to hundreds of light microscope high-power fields of view. Multiple digital images are stitched together to create a seamless ‘whole slide image’ which can be scanned in the x and y axis, and viewed dynamically through a range of magnifications (typically from 0× to 60× equivalent magnification).
Digital slide viewing software can be integrated with image editing software that facilitates digital measurement, overlay drawings, superimposed annotations and accompanying text, so that learners can view trainer-authored didactic labels and text, or add their own notes to an image. Each digital slide can be viewed by multiple learners simultaneously and accessed from anywhere in the world.
The flexibility of the digital slide medium versus the glass slide has a number of key advantages in terms of accessibility, efficiency, pedagogy and cost:

The principal disadvantage, which is particularly relevant for postgraduate learners (histopathology doctors in training), would be difficulties in obtaining key competencies in light microscope use if digital slides are the exclusive method of curriculum delivery. A balance needs to be struck between the benefits of digital pathology and the need to develop traditional microscopy skills.
Integrating Digital Slides into Undergraduate Curriculum
The place of microscopy, and indeed, of histopathology, in undergraduate medical curricula has evolved over the last few decades. Up until the early 1990s, most taught pathology modules and courses were reliant on a combination of didactic lectures and pathology case-based exercises centred on conventional light microscopy.
However, a number of curricular reforms have shifted this paradigm:
- A decrease in time allotted to pathology and basic sciences teaching in favour of increased exposure to clinical environments throughout undergraduate programmes.
- A shift from departmentally organised didactic teaching towards integrated and systems-based curricula, with more emphasis on case-based and problem-based learning and self-directed study.
- Augmentation of conventional light microscopy with digital microscopy techniques in standard clinical practice.
- Loss of multi-microscope ‘dry’ laboratories in medical schools in favour of multipurpose computer laboratories that can be used for a wider range of educational activities.
Digital slide technology has been progressively integrated into undergraduate medical, dental and allied health science curricula since the early 1990s, with digital microscopy laboratories, accessed via personal devices or in medical school-based computer laboratories gradually replacing fixed training facilities equipped with boxes of glass slides and standard optical microscopes.
Digital slides with links to additional resources, including gross macroscopic photography, radiological images and further study material, enrich the learning experience. In addition to replacing the microscopy room of pathology-rich courses, micro-doses of digital slide exposure, in the form of use of digital slides within lectures and PowerPoint slide sets, allow inclusion of histopathology content in courses that may not have previously included microscopic material.
Studies have shown that students viewing digital slides spend more time interacting with histopathology material, and perform as well or better in evaluations than their peers in fixed microscopy laboratories. Aside from large-group ‘virtual laboratory’ teachings, digital slides have been successfully incorporated into small-group learning settings too, where they can be used as part of case-based activities to encourage increased participation and a sense of community.
Empowering Postgraduate Histopathology Training
Digital slide technology has experienced a more mixed reception in the realm of postgraduate medical education. This is largely due to the lag in adoption of digital pathology for primary diagnostic practice in clinical settings. Practice differs widely from country to country and from city to city in terms of access to and usage of digital slide images for histopathology service delivery, and many departments still depend on the use of glass slides and conventional light microscopy.
Proficiency in digital pathology techniques is still not mentioned in the Accreditation Council for Graduate Medical Education Milestones requirements for trainees, and is not a core component of Royal College of Pathologists postgraduate curriculum for histopathology. The rationale for this omission is that trainees still need to balance use of digital slide technology with hands-on experience of traditional microscopy and acquisition of technical skills for glass slide diagnosis including Koehler illumination.
However, a number of online digital slide resources are available to support the learning needs of postgraduate trainees:
| Resource | Description |
|---|---|
| Shared educational slide collections | Curated web-based collections of digital slides that can be accessed by trainees in departments that do not use digital slides as part of clinical practice. |
| Live patient case archives | In departments with an evolving clinical archive of ‘live’ patient cases, trainers can direct trainees to the most relevant digital cases for that specific trainee, and share their current ‘real-world’ workload with the trainee. |
| Online CPD events | Topography specific, online continuing professional development (CPD) events that stream digital slides online, and have successfully incorporated digital slide-based pre-event and post-event self-assessment cases to consolidate learning. |
| External quality assurance materials | In the UK, external quality assurance materials have been shared in the format of digital slides, hosted by the University of Leeds Virtual Pathology website, allowing hundreds of pathologists to share rare, informative cases for discussion and consensus review. |
To be effective, educational digital slides should be interesting, challenging and authentic, and care should be taken to ensure that the level of difficulty and complexity of cases match the learning needs of participants. Clear, unambiguous examples of common pathologies should be presented for medical undergraduates, while more advanced learners, including pathology trainees, should be presented with cases of increasing rarity and difficulty, as well as ‘normal’ slides and slides with dual pathologies or unusual features.

Tuning the level of difficulty of the digital slides allows the learner to explore their personal zone of proximal development – the difference between what they can achieve without the ‘scaffolding’ of prompts or annotations and what they can do with this extra assistance. This process of scaffolding leads to increased learning, and allows for a more personalised, bespoke approach to learning, where the learner can choose the amount of scaffolding they require in different scenarios, and opt to hide or reveal different levels of labelling and annotation.
| Learner Group | Use of Digital Slides |
|---|---|
| Undergraduates | Clear, unambiguous examples of common pathologies, with suitable interactive labels and annotations to aid identification of key features. |
| Trainees | Cases of increasing rarity and difficulty, as well as ‘normal’ slides and slides with dual pathologies or unusual features. Trainees can rate their confidence in their diagnosis and assessment of a case. |
| CPD Users | Topography specific, online CPD events that stream digital slides online, with pre-event and post-event self-assessment cases to consolidate learning. |
Leveraging Digital Slides for Case-Based Learning
Small-group teaching in undergraduate histopathology education revolves around case-based learning (CBL), where the digital patient is represented by a written case study including demographic information and clinical history, possibly accompanied by radiological findings. Digital slides are easily incorporated into these cases and allow students to gain ‘hands-on’ experience navigating through tissue to identify pathologies.
The only prerequisite is access to a laptop or desktop computer and a high-speed internet connection, so CBL can be conducted remotely or in person using IT laboratory facilities. CBL has been shown to promote the development of analytical thinking skills by engaging students in discussion about complex, real-life scenarios.
CBL can also be used for postgraduate training of histopathology trainees, where it can be useful in small-group teaching settings to allow students to explore clinic–pathological correlation and how the medical context can affect the histopathological differential diagnosis. Digital slides should be presented alongside relevant medical history and multidisciplinary assessment.
Unlike undergraduate students, postgraduate students in histopathology departments have to conduct the majority of their training individually, using self-directed techniques. CBL-type cases can be adapted to suit this training environment, with case lists and digital slide links circulated to be reviewed by learners individually and fit their clinical timetable. Cases can then be discussed at regular group meetings, led by a facilitator who ensures the most salient features of the case have been appreciated by the group, and leads discussion of ambiguous aspects of the clinical context and differential diagnosis.

Fostering Collaborative Learning and Reflective Practice
Vygotsky’s theories state that the process of knowing is affected by other people and is mediated by culture and community. It follows that all learning is a collaborative process, dependent on interactions with other members of the community. When using digital slides, learners are encouraged to build upon their existing knowledge of light microscopy if applicable, and transfer this to digital techniques, noting differences, challenges and improvements with the two different diagnostic media.
When leading a group digital slide-based learning session, it can be helpful to encourage all members of the group to share their current level of experience and comfort with digital slide use. Sharing of knowledge and perspectives in this way can help individual participants construct their understanding of both the cases being discussed and the digital slide medium that is being used.
Postgraduate and continuing medical education in histopathology is often facilitated via formal or informal Communities of Practice (CoP)—professional groups with similar experiences, beliefs and values. The sharing of digital slides from educational collections, quality assurance sets and everyday practice could form a key part of CoP interaction, via informal referrals and second opinion requests.
The integration of theory and practice is one of the key tenets of healthcare education, and reflective practice is one of the key mechanisms by which this can be achieved. Learners of all stages should be encouraged to consider how they have engaged with the digital slides and what they have learnt. This ‘reflection-on-action’ allows learners to cement their understanding and develop their knowledge base.
Reflective work often works best as a collective and collaborative activity, where diverse insights and perspectives can help shape collective values. Learners can create their own annotations on digital slides to document and reinforce their awareness of the diagnostic pathway they are following, moving from superficial to deep learning.
Expanding Access and Flexibility with Digital Slides
The flexibility and transferability of the digital slide open up new opportunities for broadening the scope of learners and educators you involve in your teaching sessions. Learners from different regions, with similar specialist learning needs, can be connected and share tailored sessions with experts from anywhere in the world! In this way, we can improve equity of access to training opportunities for junior pathologists, who are no longer limited to the training staff and materials located in a single pathology department.
Similarly, the use of digital slide training sessions which can be accessed remotely can support the needs of trainees and learners who need to work and train more flexibly. At Stanley Park High School, we were able to maintain training throughout periods of COVID-19 lockdown, and offer learning opportunities to trainees and trainers who were having to isolate, shield or take on increased caring responsibilities during the pandemic.
One approach would be for trainers to assign links to digital slide cases and meet with small groups of trainees via Microsoft Teams meetings to share desktops, demonstrate how they approached the case and discuss their diagnoses. Trainers are then able to take control of the trainee case and redirect attention to particular features where necessary.
Balancing Digital and Traditional Training
Digital slides offer a practical and creative approach to histopathology training, but it is important to remember that they should be used as an adjunct to, rather than a replacement for, immersive training using standard glass slide workloads and workflow. Authentic, real-world workplace-based learning, centred around shadowing a consultant trainer and exposing the trainee to some of the more pragmatic issues around contributing to a live clinical service, is a vital part of postgraduate histopathology training.
This is the best environment for what Eraut describes as the implicit and tacit learning that occurs in the absence of overt teaching. In histopathology practice, this includes knowledge of contexts and organisations acquired through socialisation and participation. These include understanding of people and situations. The ideal training programme incorporates a range of real-world experience and curated, personalised educational content.
Conclusion
In this document, we have reviewed some of the use of digital slides for a range of learners. Digital slides represent a flexible, adaptable medium for histopathology education which can be tailored to support the needs of multiple synchronous or asynchronous learners, and can connect trainers and learners across geographical and temporal boundaries.
Digital slides, supplemented with annotation software, yield a number of pedagogical advantages over glass slides, and provide a means for efficient integration of histopathology into undergraduate curricula, a support for postgraduate trainees, and a flexible approach to continuing professional education for senior clinicians. As digital slide technology becomes more prevalent in clinical practice, the role of the digital slide in postgraduate education will be augmented. Future educational tools and programmes incorporating virtual and augmented reality technology might build upon the innate versatility of the digital slide image.

