The Pivotal Role of B Cells in the Fight Against Cancer
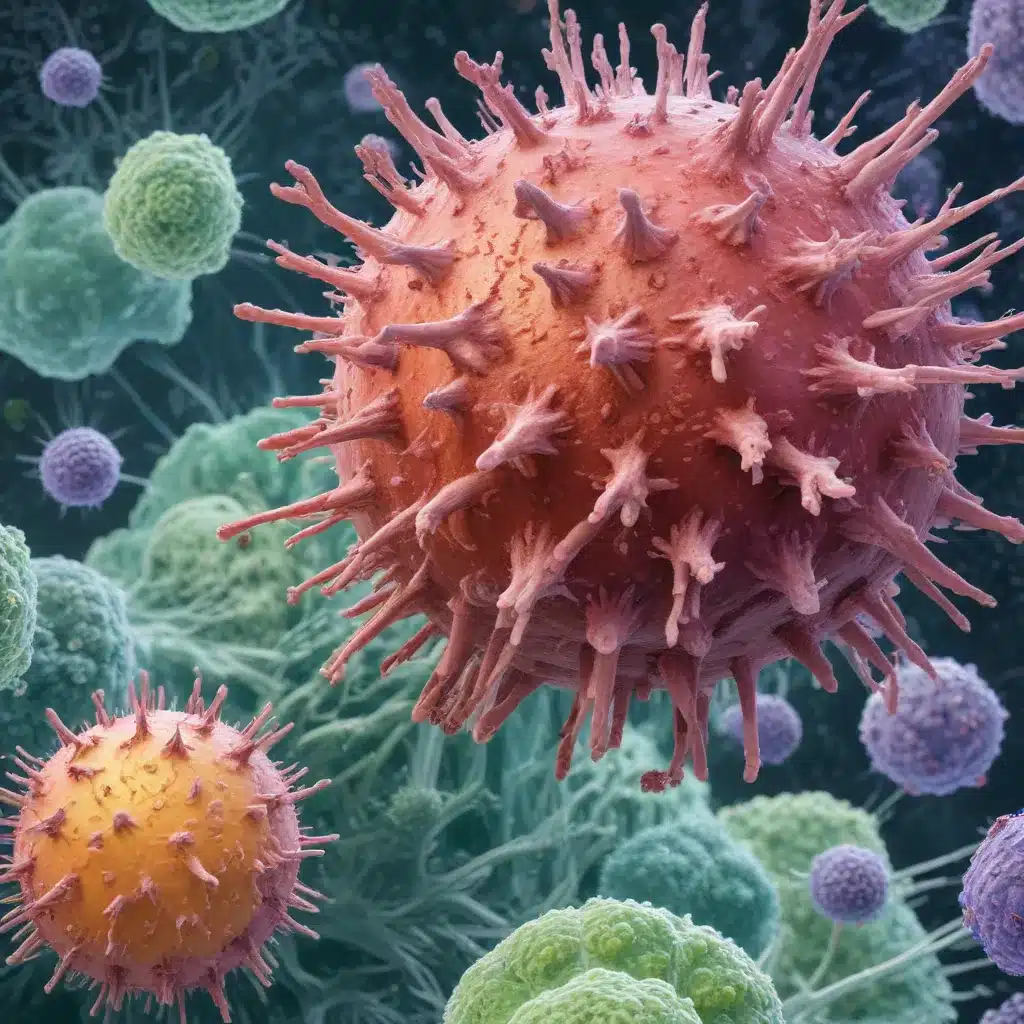
The immune system is a complex and intricate network of cells and molecules that work together to protect the body from harmful pathogens and diseases, including cancer. While the critical role of T cells in anti-tumor immunity has been well-established, the field of cancer immunotherapy is now turning its attention to the untapped potential of B cells and plasma cells (collectively known as tumor-infiltrating B lymphocytes or TIL-Bs).
Contrary to the long-held belief that B cells play a secondary role in cancer, recent studies have shown that TIL-Bs can have a significant impact on the course of the disease. In fact, the presence of TIL-Bs is associated with a positive prognosis in many cancer types, often enhancing the beneficial effects of tumor-infiltrating T cells. This suggests that B cells and their antibody-producing counterparts, plasma cells, are integral components of a robust anti-cancer immune response.
Uncovering the Diverse Phenotypes of Tumor-Infiltrating B Cells
The advent of advanced techniques, such as high-dimensional flow cytometry and single-cell RNA sequencing, has revolutionized our understanding of TIL-B phenotypes. These studies have revealed a remarkable diversity within the B cell compartment, with TIL-Bs exhibiting a wide range of developmental and functional states, from naive B cells to memory B cells and plasma cells.
Interestingly, some TIL-B phenotypes, such as the double-negative B cells (lacking expression of IgD and CD27) and the exhausted TIL-Bs (characterized by CD69+CD27-CD21- expression), have been previously associated with autoimmune conditions. This suggests that the tumor microenvironment may disrupt the delicate balance of B cell tolerance, leading to the activation of self-reactive B cells and the potential for autoimmunity-like responses against the tumor.
The Architectural Landscape of Tumor-Infiltrating B Cells
TIL-Bs can be found in distinct structural zones within the tumor microenvironment, each with its own unique features and implications for anti-tumor immunity.
Tertiary Lymphoid Structures (TLSs)
TLSs are lymph node-like structures that arise de novo within the tumor stroma in response to persistent antigenic stimuli. These organized lymphoid aggregates often contain germinal centers, where B cells undergo somatic hypermutation and affinity maturation, ultimately differentiating into high-affinity, class-switched memory B cells and plasma cells. The presence of TLSs with active germinal centers is a strong predictor of favorable clinical outcomes, underscoring the importance of B cell-mediated responses in shaping the anti-tumor immune landscape.
Lympho-Myeloid Aggregates (LMAs)
In addition to the highly organized TLSs, TIL-Bs can also be found in less structured stromal infiltrates, which we refer to as lympho-myeloid aggregates (LMAs). These infiltrates typically comprise a mix of B cells, T cells, and myeloid cells, suggesting a collaborative effort in mediating anti-tumor immunity.
Intra-Epithelial Infiltrates
TIL-Bs can also be found within the tumor epithelium, where they come into direct contact with cancer cells. The significance of these intra-epithelial B cell infiltrates is not yet fully understood, but they may play a role in direct cytotoxicity or in facilitating interactions between B cells, T cells, and myeloid cells within the tumor.
The Antigen Specificity of Tumor-Infiltrating B Cells
A critical question in the field of cancer immunology is the nature of the antigens recognized by TIL-Bs. Unlike tumor-reactive T cells, which often target mutated, cancer-specific neoantigens, TIL-Bs appear to predominantly recognize self-antigens with varying degrees of tumor-specific expression.
This observation raises fascinating immunological questions, as B cells and T cells employ distinct tolerance mechanisms. While T cells are primarily tolerized to foreign (non-self) antigens, B cells must also maintain tolerance to a broad array of self-antigens. The fact that TIL-Bs can recognize self-antigens suggests that the tumor microenvironment may disrupt peripheral B cell tolerance mechanisms, akin to what is observed in autoimmune disorders.
Interestingly, a small number of TIL-Bs have been found to target viral antigens, such as those derived from human papillomavirus (HPV), or mutated proteins, like the tumor suppressor p53. These findings highlight the potential for TIL-Bs to recognize both self-antigens and tumor-specific neoantigens, presenting a diverse array of targets for potential therapeutic exploitation.
The Effector Mechanisms of Tumor-Infiltrating B Cells
TIL-Bs possess a versatile arsenal of effector mechanisms that can contribute to anti-tumor immunity. In addition to their well-known role in producing antigen-specific antibodies, TIL-Bs can also:
-
Enhance Adaptive Immune Responses: TIL-Bs can act as antigen-presenting cells, effectively priming and activating tumor-specific T cells. They can also recruit and support other immune cells, such as T cells and natural killer cells, through the production of chemokines and cytokines.
-
Activate Innate Immune Mechanisms: TIL-Bs can engage the complement system, leading to direct lysis of tumor cells or the recruitment of other immune effector cells. They can also stimulate antibody-dependent cellular cytotoxicity (ADCC) and phagocytosis by myeloid cells.
-
Combat Immune Evasion: The antibodies produced by TIL-Bs can neutralize immunosuppressive factors, such as transforming growth factor-beta (TGF-β), or block immune checkpoint molecules, like programmed cell death protein 1 (PD-1) and its ligand, PD-L1.
-
Regulate the Tumor Microenvironment: TIL-Bs can directly kill tumor cells through the production of granzyme B and other cytotoxic molecules. They can also modulate the tumor stroma and vasculature, thereby influencing the overall tumor microenvironment.
-
Promote Immunological Memory: The formation of long-lived, high-affinity memory B cells and plasma cells within TLSs can provide durable, antigen-specific protection against tumor recurrence.
The multifaceted effector capabilities of TIL-Bs highlight their potential to complement and synergize with other immune-based therapies, such as checkpoint inhibitors and adoptive T cell transfer, to enhance the reach, potency, and durability of cancer immunotherapy.
Harnessing the Power of B Cells in Cancer Immunotherapy
Given the promising role of TIL-Bs in shaping anti-tumor immunity, researchers and clinicians are actively exploring strategies to harness their unique capabilities in the fight against cancer. Some of the most promising approaches include:
-
Enhancing TIL-B Responses: Interventions that promote the recruitment, activation, and differentiation of TIL-Bs, such as the modulation of B cell-activating factors (e.g., BAFF, IL-21) or the targeting of inhibitory pathways (e.g., Fc gamma receptor IIB, PD-1/PD-L1).
-
Exploiting TIL-B Effector Functions: Leveraging the antibody-mediated effector functions of TIL-Bs, either through the use of therapeutic monoclonal antibodies or by stimulating the production of tumor-specific antibodies.
-
Combining TIL-B-Targeted Therapies with other Immunotherapies: Integrating TIL-B-focused strategies with established approaches, such as checkpoint inhibitors, adoptive T cell transfer, and cancer vaccines, to create synergistic anti-tumor effects.
-
Targeting Regulatory B Cells: Identifying and neutralizing the immunosuppressive activities of Breg cells within the tumor microenvironment to unleash the full potential of effector TIL-Bs.
-
Addressing Autoimmunity Concerns: Carefully monitoring and managing the potential for autoimmune-like responses associated with the disruption of B cell tolerance mechanisms.
As the field of cancer immunotherapy continues to evolve, the integration of TIL-B-targeted strategies into comprehensive treatment approaches holds great promise for extending the reach, potency, and durability of anti-cancer immune responses. By harnessing the power of B cells, we can unlock new avenues for improving outcomes for patients with a wide range of malignancies.
To learn more about the latest developments in cancer immunotherapy and how you can get involved, visit the Stanley Park High School website.

