Understanding the Role of LDHB in Breast Cancer
Breast cancer is one of the most common and devastating forms of cancer affecting women worldwide. As an experienced educational writer, I’m pleased to provide an in-depth exploration of the critical role that lactate dehydrogenase B (LDHB) plays in shaping the tumor microenvironment and influencing the body’s immune response to breast cancer.
The Metabolic Landscape of Breast Cancer
Cancer cells are known for their ability to rapidly proliferate and evade the body’s natural defenses. At the heart of this process lies a fundamental shift in the way cancer cells metabolize nutrients, a phenomenon known as the “Warburg effect.” Instead of relying on the efficient process of oxidative phosphorylation to generate energy, breast cancer cells preferentially convert glucose to lactate through a less efficient process called glycolysis.
This metabolic reprogramming allows cancer cells to quickly generate the ATP they need to support their rapid growth. However, it also results in the accumulation of lactic acid, which can have a detrimental impact on the tumor microenvironment and the body’s anti-cancer immune response.
The Crucial Role of LDHB
Lactate dehydrogenase (LDH) is a key enzyme that plays a central role in this metabolic shift. LDH catalyzes the interconversion of pyruvate and lactate, and it exists in various isoforms, including LDHA and LDHB. While LDHA primarily drives the conversion of pyruvate to lactate, LDHB is responsible for the reverse reaction, converting lactate back into pyruvate.
Recent studies have revealed that the expression of LDHB is often decreased in breast tumor cells. This downregulation of LDHB has important implications for the tumor microenvironment and the body’s immune response.
Decreased LDHB Leads to Immune Dysfunction
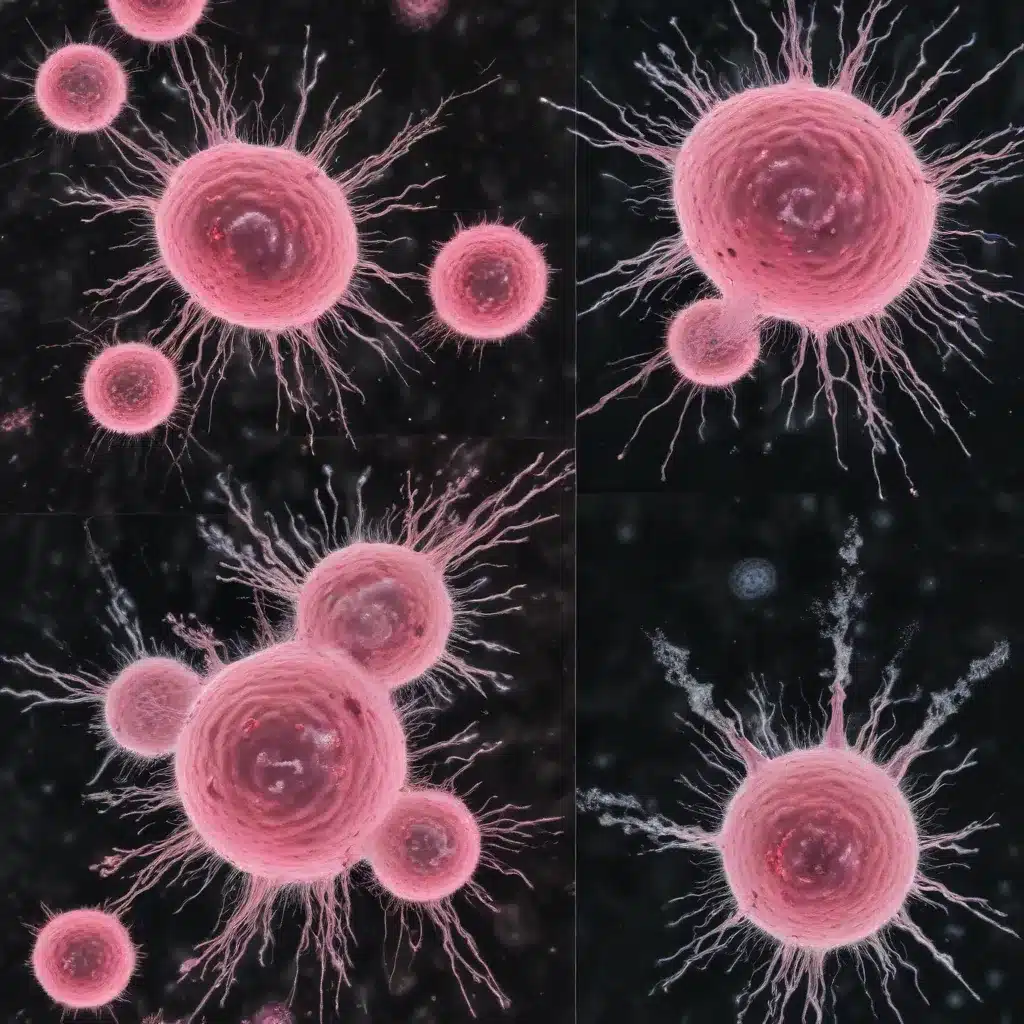
When LDHB expression is low in breast tumor cells, the resulting accumulation of lactic acid in the tumor microenvironment can have a profound impact on the activity and function of natural killer (NK) cells. NK cells are a crucial component of the body’s anti-cancer immune response, as they are capable of directly killing tumor cells.
However, the high levels of lactic acid in the tumor microenvironment can impair the ability of NK cells to effectively recognize and eliminate breast cancer cells. This impairment of NK cell function can contribute to the progression of breast cancer and the poor prognosis associated with decreased LDHB expression.
Restoring LDHB Expression Enhances Anti-Tumor Immunity
Interestingly, studies have shown that restoring LDHB expression in breast tumor cells can help to reverse this immune dysfunction. By increasing the expression of LDHB, the levels of lactic acid in the tumor microenvironment are reduced, allowing NK cells to regain their cytotoxic activity and effectively target and destroy breast cancer cells.
This finding suggests that targeting the LDHB-mediated regulation of the tumor microenvironment could be a promising avenue for the development of new breast cancer therapies. By enhancing the body’s natural immune response against breast cancer, these strategies have the potential to improve patient outcomes and reduce the burden of this devastating disease.
The Impact of LDHB on Breast Cancer Prognosis
The association between LDHB expression and breast cancer prognosis is a crucial aspect of understanding the role of this enzyme in the disease. Numerous studies have consistently demonstrated that decreased LDHB expression in breast tumor cells is linked to a poorer overall prognosis for patients.
Linking LDHB to Immune Cell Infiltration and Activation
One of the key reasons for this connection between LDHB and prognosis is the enzyme’s impact on the tumor microenvironment and the immune response. As mentioned earlier, decreased LDHB expression leads to the accumulation of lactic acid, which can impair the function of NK cells and other important immune cells.
Interestingly, analyses of breast cancer patient samples have shown that tumors with higher LDHB expression tend to have increased infiltration and activation of various immune cell populations, including NK cells, T cells, and dendritic cells. This enhanced immune cell presence and activity within the tumor microenvironment is associated with better clinical outcomes for patients.
LDHB as a Potential Biomarker and Therapeutic Target
Given the strong link between LDHB expression and breast cancer prognosis, researchers have explored the potential of using LDHB as a biomarker to predict patient outcomes and guide treatment decisions. By assessing the levels of LDHB in breast tumor samples, healthcare providers may be able to identify patients who are at a higher risk of disease progression and poor outcomes.
Moreover, the ability of LDHB to modulate the tumor microenvironment and enhance the anti-tumor immune response suggests that targeting this enzyme could be a promising therapeutic approach. By developing strategies to restore or maintain LDHB expression in breast tumor cells, it may be possible to boost the body’s natural defenses against the disease and improve overall patient survival.
Harnessing the Power of the Immune System
The crucial role of LDHB in shaping the tumor microenvironment and influencing the body’s immune response to breast cancer highlights the importance of understanding the complex interplay between cancer metabolism and the immune system.
Activating NK Cells to Fight Breast Cancer
As discussed, the downregulation of LDHB in breast tumor cells can lead to the accumulation of lactic acid, which in turn impairs the function of NK cells. By restoring LDHB expression and reducing lactic acid levels, it may be possible to reinvigorate the cytotoxic activity of NK cells, allowing them to more effectively recognize and eliminate breast cancer cells.
This approach of harnessing the power of the immune system to combat breast cancer is particularly promising, as it offers the potential to target the disease in a more targeted and personalized manner, without the harmful side effects often associated with traditional cancer therapies.
Integrating Metabolic Regulation and Immunotherapy
The connection between LDHB and the tumor microenvironment also suggests that strategies to modulate cancer metabolism could be effectively combined with immunotherapeutic approaches to enhance the body’s anti-cancer defenses.
For example, by developing therapies that target the enzymes involved in the Warburg effect, such as LDHB, it may be possible to create a more favorable microenvironment for the proliferation and activation of anti-tumor immune cells. This synergistic approach could potentially lead to improved patient outcomes and a more effective long-term control of breast cancer.
Conclusion: A Promising Path Forward
The insights gained from the research on LDHB and its role in breast cancer have opened up new avenues for understanding the complex interplay between cancer metabolism and the immune response. By harnessing this knowledge, healthcare providers and researchers can work towards developing more targeted and effective strategies to combat this devastating disease.
As a school community, we encourage you to stay informed about the latest developments in breast cancer research and to support ongoing efforts to improve patient outcomes. By working together, we can empower individuals to take an active role in their health and contribute to the fight against breast cancer.
For more information on breast cancer and the latest advancements in research and treatment, please visit the Stanley Park High School website. We are committed to providing our students and their families with the resources and support they need to navigate this complex landscape and make informed decisions about their health.

