Understanding the Diverse Presentation of Amyotrophic Lateral Sclerosis
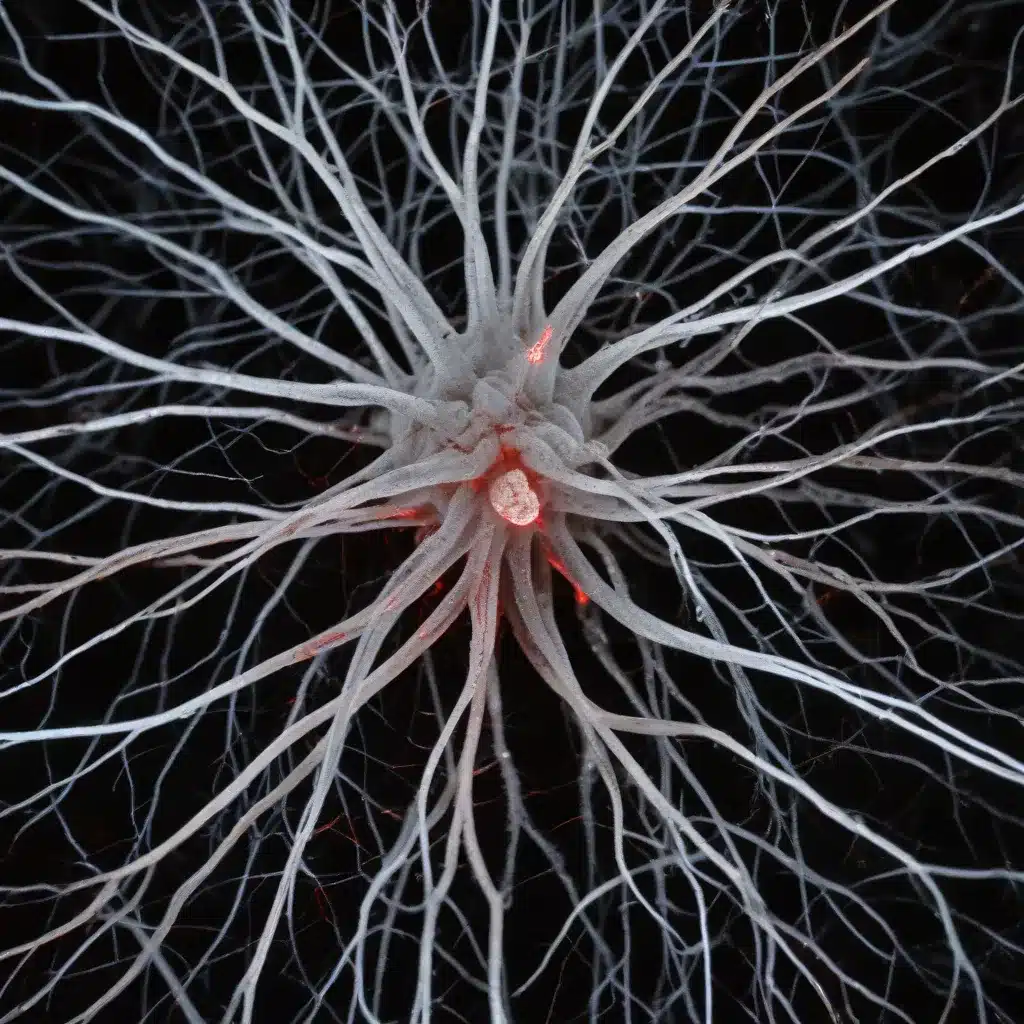
Amyotrophic Lateral Sclerosis (ALS) is a devastating neurodegenerative disease that affects the motor neurons, leading to progressive muscle weakness and paralysis. One of the hallmarks of ALS is its marked clinical heterogeneity, with a wide range of motor presentations and disease trajectories. While the coexistence of upper and lower motor neuron signs is common, some patients exhibit atypical motor symptoms that challenge our understanding of the underlying pathogenic mechanisms.
Emerging research suggests that the dysfunction of the motor cortex, specifically the corticomotoneuronal system, may be a crucial factor in shaping the clinical phenotype of ALS. Transcranial Magnetic Stimulation (TMS) has emerged as a valuable tool to explore the in vivo excitability of the motor cortex, revealing distinct cortical excitability profiles across different ALS subgroups.
In this comprehensive article, we will delve into the fascinating insights uncovered by a recent study that investigated the relationship between cortical inexcitability, a less-studied feature of upper motor neuron (UMN) dysfunction in ALS, and the clinical presentation of the disease. By understanding the correlations between this specific cortical signature and the ALS phenotype, we can gain valuable clues about the underlying disease mechanisms and explore the implications for patient management and clinical trial design.
Identifying Cortical Inexcitability in ALS
The study, published in the Journal of Neurology, Neurosurgery, and Psychiatry, recruited a large cross-sectional cohort of 417 ALS patients and utilized the threshold-tracking TMS technique to differentiate them into three distinct groups:
- Inexcitable: Patients who exhibited no TMS response at maximal stimulator output, despite preserved lower motor neuron (LMN) function.
- Hyperexcitable: Patients with short interval intracortical inhibition (SICI) ≤ 5.5%, indicating cortical hyperexcitability.
- Normal Cortical Excitability: Patients with SICI > 5.5%, exhibiting normal cortical excitability.
Remarkably, the study found that a significant proportion (26.4%) of the ALS cohort exhibited cortical inexcitability, a finding that challenges the traditional understanding of ALS pathophysiology.
Distinguishing the Cortical Inexcitability Phenotype
When the researchers delved deeper into the characteristics of the cortical inexcitability group, several intriguing differences emerged compared to the hyperexcitable and normal excitability cohorts:
Younger Age of Onset
Patients with cortical inexcitability were significantly younger at the time of disease onset, with a mean age of 58.2 years, compared to 62.9 years in the hyperexcitable group and 60.6 years in the normal excitability group.
More Prominent Upper Motor Neuron Signs
The cortical inexcitability group exhibited more pronounced upper motor neuron (UMN) signs, as evidenced by significantly higher UMN scores compared to the other two groups. This suggests a greater degree of corticomotoneuronal dysfunction in this subgroup.
Greater Functional Decline
Patients with cortical inexcitability experienced more severe functional impairment, as indicated by significantly lower scores on the Revised Amyotrophic Lateral Sclerosis Functional Rating Scale (ALSFRS-R). This highlights the profound impact of cortical inexcitability on the overall disease course and quality of life.
Predominant Upper Limb Weakness
The study found that the cortical inexcitability group displayed more prominent upper limb weakness, particularly in the dominant right hand. This was evidenced by significantly reduced upper limb strength scores compared to the other groups, suggesting a specific vulnerability of the motor cortical representation and corticospinal tract involvement in this subpopulation.
More Advanced Disease Stage
Interestingly, a greater proportion of patients with cortical inexcitability were classified as having Awaji probable or definite ALS, indicating more advanced disease dissemination. Furthermore, these patients showed higher King’s staging scores, reflecting greater clinical disease spread.
Delayed Diagnosis
The study also revealed that patients with cortical inexcitability were less likely to be on riluzole, a medication commonly prescribed for ALS, at the time of assessment. This suggests a potential delay in diagnosis for this subgroup, potentially due to the atypical clinical presentation.
Implications for Understanding ALS Pathophysiology
The findings of this study offer valuable insights into the complex pathophysiology of ALS and the role of cortical dysfunction in shaping the clinical phenotype.
The initial reduction in motor thresholds and cortical hyperexcitability observed in early-stage ALS may reflect a state of motor neuron hyperexcitability, potentially driven by compensatory mechanisms or underlying pathological processes. As the disease progresses, however, the degeneration or dysfunction of corticomotoneurons and their associated interneuronal circuits can lead to increased motor thresholds and ultimately, cortical inexcitability.
The presence of cortical inexcitability in a substantial proportion of the ALS cohort suggests that this may represent a distinct pathological pathway, potentially driven by selective vulnerability within the motor cortex. The younger age of onset, more prominent UMN signs, and greater functional decline observed in this group may indicate an ALS subtype with a predominant upper motor neuron involvement, akin to the primary lateral sclerosis (PLS) phenotype.
However, the survival outcomes in the cortical inexcitability group were comparable to the other ALS subgroups, suggesting that the younger age of this cohort may confer a survival advantage that offsets the more advanced disease stage and greater functional impairment.
Implications for Patient Care and Clinical Trials
The identification of the cortical inexcitability phenotype has important implications for the management and clinical trial design in ALS.
From a patient care perspective, the recognition of this specific ALS subtype should prompt a tailored approach to rehabilitation and supportive strategies. The more prominent upper limb weakness and greater functional decline observed in this group may require a greater emphasis on occupational therapy, assistive devices, and strategies to optimize quality of life.
Furthermore, the potential for diagnostic delay in this subgroup highlights the importance of considering cortical excitability profiles as part of the diagnostic workup in suspected ALS cases. Incorporating TMS assessments into the clinical evaluation may aid in the early identification of this distinct phenotype, leading to more timely interventions and improved patient outcomes.
In the context of clinical trials, the presence of cortical inexcitability may serve as an important stratification factor in patient selection. Given the unique clinical features and disease trajectory of this subgroup, their inclusion or exclusion from clinical trials could impact the interpretation of study outcomes. Incorporating TMS parameters as biomarkers in trial designs may also help elucidate the role of cortical dysfunction in disease progression and response to novel therapies.
Conclusion
The comprehensive study on cortical inexcitability in ALS has unveiled a compelling and previously underappreciated clinical phenotype. By shedding light on the diverse manifestations of ALS, this research underscores the importance of exploring the motor cortex’s role in shaping the clinical presentation of the disease.
As we continue to unravel the complex pathophysiology of ALS, the insights gained from this study will be invaluable in guiding patient management, informing clinical trial design, and ultimately, advancing our understanding of this devastating condition. By recognizing and addressing the unique needs of the cortical inexcitability subgroup, we can strive to provide more personalized and effective care for individuals living with ALS.
For more information on ALS and the latest research, we encourage you to visit the Stanley Park High School website. Our dedicated community is committed to supporting individuals and families affected by this condition, and we are proud to share these important findings with our school community.

