The global threat of antimicrobial resistance
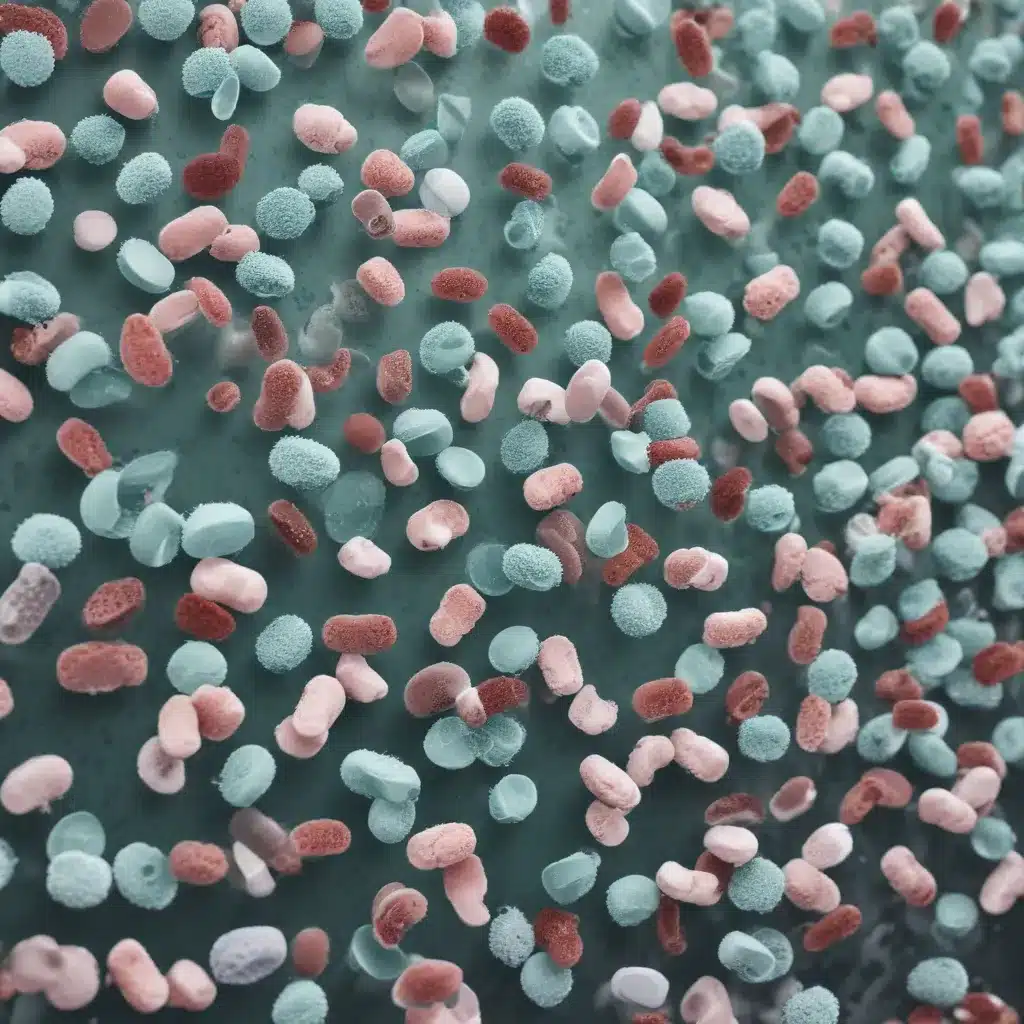
Antimicrobial resistance (AMR) is one of the biggest public health challenges the world faces today. As bacteria, viruses, fungi and parasites evolve to resist the medicines used to treat the infections they cause, it is becoming increasingly difficult to ensure effective prevention and treatment. This poses a grave threat to human, animal and environmental health across the globe.
The scale of the AMR problem is staggering. In the European Union and European Economic Area (EU/EEA) alone, antibiotic-resistant infections resulted in over 38,000 deaths and more than 1 million years of life lost in 2019. Globally, it’s estimated that drug-resistant infections could cause 10 million deaths per year by 2050 if action is not taken. The economic impact is also severe, with the EU facing additional healthcare costs of around €1.1 billion annually.
Tackling AMR requires a comprehensive, cross-sectoral ‘One Health’ approach that addresses the interconnected human, animal and environmental factors driving resistance. This is a complex challenge that demands coordinated efforts from governments, health systems, researchers, industry and the public. Developing and implementing effective national action plans (NAPs) to combat AMR is crucial, but progress has been uneven across countries.
Antimicrobial resistance in Argentina: progress and challenges
Argentina has been a leader in the Latin American region when it comes to addressing AMR. The country implemented its first national action plan to tackle AMR in 2015, and has since made important strides in areas like antibiotic regulation, surveillance, and stewardship.
For example, Argentina introduced a gradual ban on the use of the antibiotic colistin in food-producing animals starting in 2019. It has also prohibited the use of antibiotics as growth promoters in livestock. And the country has established a robust national surveillance system for monitoring antibiotic consumption and resistance rates in hospitals.
However, Argentina still faces significant challenges in fully implementing its AMR action plan and strengthening its One Health approach to the issue. A recent study found that the country’s efforts in areas like accountability, monitoring and evaluation, and policy design could be improved. Gaps remain in areas like cross-coordination between stakeholders, access to diagnostics and treatment in different regions, and surveillance of AMR in the food production and environmental sectors.
Addressing these challenges will be crucial for Argentina to make further progress in tackling the growing threat of drug-resistant infections. The country’s experience provides valuable lessons for other nations seeking to strengthen their own national strategies and policies on AMR.
Opportunities and challenges in Argentina’s AMR governance
A recent in-depth study conducted in Argentina shed light on the key opportunities and challenges the country faces in implementing its national action plan on AMR. Researchers interviewed a range of stakeholders from government, academia, the private sector, and civil society to understand their perspectives on the progress, barriers and future priorities for AMR policy and control.
Cultural factors and country context
One of the overarching themes that emerged was the impact of Argentina’s unique cultural and socio-political context on AMR efforts. Participants described how the country’s frequent economic and political shifts, including shortages and high inflation, have destabilized the healthcare system and made it challenging to ensure sustainable AMR control measures.
“Argentina has 30 years of experience on AMR surveillance, we live economic shortages and political shifts fiercely in Argentina; a state of crisis, and we are somewhat used to this dynamic trying to cope with it as best we can. We have developed good coordinating links between teams centralised on good communication skills, but we cannot guarantee sustainability. It will depend on future leader’s coordination since monetary resources are limited, a lot relies upon the projects or people’s willingness to contribute but we believe it will perpetuate.” – Participant from a public institution
Participants also highlighted how deep-rooted cultural norms and values, such as a preference for quick fixes and self-medication, pose barriers to changing behaviors around antibiotic use, especially in the agricultural sector. Shifting these entrenched attitudes will be crucial but extremely challenging.
“Inappropriate antibiotic use, driven by cultural norms like self-medication and seeking quick remedies is often influenced by limited healthcare access. This extends into food production, where profit motives can override caution. A shift in cultural perspective is crucial, educating on responsible use and the benefits of animal welfare and sustainable practices across the sectors.” – Participant from a public institution
Fragmented governance and coordination
Another key challenge identified was the fragmented nature of Argentina’s administrative and governance structures when it comes to AMR. While the country’s National Commission for the Control of Antimicrobial Resistance (CoNaCRA) plays a central coordinating role, there are gaps in alignment and accountability between national, provincial and local levels of government.
“There is a problem with the administration system that limits or enhances the ability to perform improvements towards tackling AMR. SENASA conducts extensive and well-articulated labour; however, the lack of auditing and accountability in decentralised administrations (regions) in Argentina hampers AMR control due to the inherent variability in the quality of care and health access.” – Participant from a public institution
Participants noted that while communication and relationships between stakeholders are generally strong, there is a need for more integrated, cross-sectoral decision-making and information-sharing. Developing robust horizontal linkages between the human health, animal health and environmental sectors will be crucial for a comprehensive One Health approach.
“The NAP has significantly advanced and enhanced interdisciplinary and interdepartmental cooperation between animal and human health sectors, primarily driven by the CoNaCRA, which has facilitated knowledge sharing. However, the challenge of synchronising NAP initiatives across 24 distinct provinces in a federal system underscores the imperative for more effective inter- and intra-level cooperation.” – Participant from a public institution
Antibiotic access, use and regulation
Access to and use of antibiotics emerged as another key area of focus, with participants highlighting both positives and negatives. On the human health side, antibiotic access and stewardship are relatively well-regulated, with hospitals and laboratories working collaboratively. However, issues remain around mandatory prescription requirements not being fully enforced, and the sale of antibiotics in dosages greater than needed.
In the animal sector, the picture is more fragmented. Veterinarians do not always closely monitor antibiotic purchasing, application and storage, and local regulations are limited. This can lead to inappropriate and excessive use, which fuels the development of resistance.
“Antibiotics are still sold without a prescription either for human or animal use (more frequent among animals), even if prescriptions are mandatory by law, including keeping track of their usage by health professionals (electronic sales). Another issue is the dosage; antibiotics are usually sold in dosages greater than needed, which incentivises inappropriate utilisation maximising commercial interests.” – Participant from academia
At the same time, participants were optimistic about the potential for alternatives to antibiotics, such as vaccines, feed additives and plant-based compounds, to reduce antibiotic use in food production.
Awareness and surveillance
While awareness of AMR and its health impacts has grown, especially among key institutions, participants felt that public awareness campaigns have had limited reach. There are also gaps in knowledge and understanding around antibiotic use and resistance, particularly among veterinarians and agricultural producers.
“There is a problem with vets’ knowledge of antibiotics, specifically in terms of pharmacokinetic and pharmacodynamic aspects, the correct calculation of the dose administration. It is the duration of treatment in the form of clinical criteria and corresponding to specific physiological situations. All these aspects are related to rational antibiotic usage. If you forget these aspects, you can reach a therapeutic failure despite having chosen the correct antibiotic based on what the laboratory said; and this is largely prevalent in the country.” – Veterinarian from academia
When it comes to surveillance, Argentina has made good progress, especially in the human health sector. A nationwide network of over 200 hospitals regularly monitors antibiotic resistance and consumption. But surveillance in the animal and environmental sectors lags behind, hampered by the fragmented nature of the food production industry and limited resources.
“INTA monitors some animal production chains, but surveillance is the primary task of SENASA, for example, in dairy, we evaluate animals experiencing a mastitis disease and track AMR and potential environmental reservoirs with technology developed locally. Another example, we detect Salmonella in animals and utilise microbiological analyses, including phenotyping and genotyping to analyse AMR and evolution, as part of surveillance routines hand by hand with SENASA. However, most surveillance comes from the governmental side, sampling seasonality is not often captured due to limited resources, the quantity of livestock farms is massively distributed throughout the country, and local producer’s veterinary diagnostics are often sent to private labs where traceability is missing.” – Veterinarian from a public organization
National action plan and external drivers
Despite the challenges, participants expressed a generally positive view of the progress made through Argentina’s national action plan on AMR. Initiatives like the establishment of CoNaCRA, new AMR-focused legislation, and expanded surveillance and stewardship programmes were seen as important steps forward.
However, external factors like the COVID-19 pandemic have negatively impacted AMR efforts by diverting resources and attention. The pandemic also exacerbated antibiotic misuse, as teams were “absolutely overwhelmed” and “all the artillery was dedicated to diagnosis and containment of COVID.”
At the same time, the pandemic has had some positive lessons, like highlighting the value of virtual collaboration and reinforcing the importance of personal hygiene. And Argentina has benefited from strong international partnerships and funding to support its AMR work.
“The pandemic has taught us, it’s to prioritize our personal hygiene. Hand washing and personal care help us not get sick from diseases, and if we don’t get sick, we do not require antibiotics.” – Veterinarian from a public organization
Strengthening Argentina’s AMR response
Argentina’s experience highlights both the progress that can be made in tackling AMR, as well as the significant ongoing challenges. Addressing these challenges will require a multifaceted, sustained effort that draws on the country’s strengths while overcoming deeply-rooted barriers.
Key priorities for strengthening Argentina’s AMR response include:
- Enhancing governance and accountability, including better aligning national, provincial and local initiatives and improving auditing and oversight mechanisms.
- Improving antibiotic access, use and regulation across the human health, animal health and environmental sectors through measures like better monitoring, enforcement of prescription requirements, and promotion of alternatives.
- Boosting awareness and education, targeting a wide range of stakeholders from the general public to veterinarians and agricultural producers.
- Expanding and integrating AMR surveillance, particularly in the animal and environmental domains, to get a comprehensive picture of resistance patterns and drivers.
- Ensuring the long-term sustainability and resourcing of the national action plan, including by leveraging international partnerships and funding.
Ultimately, Argentina’s experience demonstrates that tackling AMR requires a holistic, collaborative approach that addresses the complex interplay of cultural, political, economic and technical factors. As a regional leader, Argentina’s continued progress in this area can provide valuable lessons for other countries seeking to strengthen their own national strategies for combating this global health threat.
For the latest updates and resources on antimicrobial resistance, visit the Stanley Park High School website.

